The final section of the human intestine is the large intestine. It starts from the ileocecal valve and ends at the anus.
Content
Colon Anatomy
The following sections of the large intestine are distinguished:
- cecum
- ascending colon
- transverse colon
- descending colon
- sigmoid colon
- rectum.
The ascending colon forms a right hepatic bend at a right angle, less often at an acute angle, in the upper right region of the abdomen as it passes into the transverse colon. The right bend is in contact with the lower surface of the liver and the bottom of the gallbladder.
The transverse colon has a length of 25 to 62 cm and a mesentery of 12 cm. The transverse intestine hanging down can be located in the small pelvis and become the contents of the hernial sac, even with inguinal and femoral hernias.
In the left upper region of the abdomen there is the left splenic flexure at the transition of the transverse colon to the descending colon. It forms an acute angle.
The length of the colon ranges from 110 to 215 cm, the internal diameter is 5-8 cm at the beginning and decreases towards the rectum.
Unlike the small intestine, the structure of the large intestine contains ribbons, haustra and omental processes. The tapes tighten and corrugate the intestine, thereby forming haustra, niche-like protrusions of the intestinal wall. Omental processes are inclusions of fat about 5 cm long, covered with a serous membrane. Their functional purpose is unknown.
The small intestine is inserted into the cecum; at the junction there is the ileocecal valve, which, opening slightly, allows the contents of the small intestine to enter the cecum. It also prevents the contents of the colon from flowing back into the small intestine.
Position of appendicitis
The vermiform appendix (appendix) is a continuation of the cecum, its length is normally 7-8 cm, diameter 8 mm. In some cases, the length can vary from 0.5 cm to 33 cm. The process has its own mesentery, so the position of its peripheral (terminal) part can change.
The following positions of the appendix in the abdominal cavity are possible:
- the process is directed into the pelvic cavity;
- parallel to the ileum ;
- in the right lateral canal;
- ascending, when the apex may be in the subhepatic region;
- retrocecal, when the process is located behind the cecum.
The ascending colon has a length of 18-20 cm. In 5% of cases it has a mesentery and becomes mobile, which can cause volvulus, cecum and ascending.
The structure of the intestinal walls
The wall of the colon is composed of
- mucous membrane
- submucosa
- muscularis propria
- serous membrane.
The mucous membrane consists of, among other things, a large number of goblet cells that produce mucus. Mucus makes it easier for stool to move through the colon.
The submucosa contains a large number of blood and lymphatic vessels, as well as nerve fibers.
The muscular lining of the colon is significantly different from the small intestine. It consists of powerful smooth muscles, forming an inner layer of circular and outer layer of longitudinal muscle fibers. Between these layers is the nerve plexus.
There may be a bulge in the wall of the colon called a diverticulum. It can be either congenital or acquired.
The serous membrane has a number of features in its structure. On its surface there are omental processes 4-5 cm long, filled with fatty tissue. These processes are capable of twisting, which can lead to necrosis and symptoms of an acute abdomen.
Sphincters of the colon
The presence of a large number of physiological sphincters in the colon ensures its motility.
The ileocecal sphincter of Varolius is located at the junction of the ileum and the cecum.
The colocecal sphincter of Busi separates the cecum and ascending colon.
Geertz's sphincter is located on the border of the middle and upper third of the ascending colon.
The right and left Kenon sphincters are located, respectively, near the right and left bends of the transverse colon.
Horst's sphincter is located in the middle third of the transverse colon.
The sphincters of Pyra and Bally limit the descending meningeal colon above and below.
The Rossi-Moutier sphincter is located in the middle third of the sigmoid colon.
The Auburn-Pirogov-Muthier sphincter is in the last third of this intestine.
Sphincters are wide folds that are closed in the normal state and straighten during peristalsis.
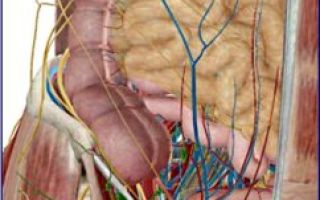
Blood supply of the large intestine
The intestinal blood supply comes from two mesenteric arteries - superior and inferior. The large intestine is supplied with blood by the superior mesenteric artery to the left flexure. The inferior mesenteric supplies blood to the left parts of the colon.
The distribution of blood to all parts of the intestine is carried out by straight vessels, which arise from a parallel vessel running along the entire mesenteric edge.
Along with the arteries there are veins and lymph nodes of the same name.
With mesentral insufficiency of the inferior mesenteric artery, areas of the colon are affected, in 80% of cases in the area of the left flexure. This leads to the development of ischemic colitis.
Colon motility
Various parts of the nervous system are involved in ensuring colon motility.
Sensory fibers of the spinal nerves and the vagus nerve provide sensory innervation to the intestines. The motor function of the intestine is provided by the autonomic nervous system.
The final function of the intestine is provided by the rectum.
Functions of the large intestine
During the digestion process, the large intestine performs a number of important functions:
- suction
- mechanical
- endocrine
- immune.
Suction
In the large intestine, water and salts are absorbed from the food mass (chyme). As a result, the chyme becomes dehydrated and turns into feces. In contrast to absorption, colonic secretion occurs. The intestinal secretion secreted by the mucous membrane has a liquid consistency and an alkaline reaction. Sometimes the pH of the colon exceeds 9.0.
Regulation of absorption and secretion is carried out by the autonomic nervous system, endocrine and neuropeptide systems, which are in complex interaction with each other.
Digestion in the large intestine
The large intestine is a reservoir of microflora. Normal microflora performs a number of vital functions:
- produces antibodies that protect against pathogenic bacteria,
- participates in the synthesis of vitamins C, B, PP, folic and pantothenic acids,
- participates in the metabolism of fat-soluble vitamins A, D, E, K,
- breaks down fiber
- participates in the hydrolysis of proteins, fats, carbohydrates,
- regulates the absorption of microelements - calcium, iron, magnesium, phosphorus.
There are a huge number of microorganisms in the colon. They utilize the remaining undigested components. Organic acids, carbon dioxide, methane, hydrogen sulfide, and toxic substances released as a result of decay processes under the influence of microbes are absorbed and neutralized by the liver.
Mechanical function
The large intestine pushes the contents (stool) distally and carries them out.
The cecum receives 300-500 ml of chyme daily with the remains of undigested food. Stirring movements mix the contents of the intestine, resulting in slow absorption of water. Through three or four massive contractions, this content is moved into the descending colon and into the rectum.
In the transverse colon, circular contractions mix the intestinal contents and make them harder.
In the sigmoid colon, slow contractive movements occur with a frequency of 20-30 s. The contraction phase gives way to a resting phase.
Studies have shown that 1-10 minutes after eating, a periodic increase in activity occurs, which is accompanied by intense motility and mucous secretion. This motor activity involves simultaneous contraction of all segments of the colon. Peristaltic waves of large movements of the colon usually reach the rectum. Filling of the rectum with feces causes stretching of its wall and the urge to defecate.
Endocrine function
The epithelium of the colon contains cells of the diffuse endocrine system. These cells produce hormones that regulate both the activity of the intestines and the body as a whole.
Immune function
This function is provided by diffuse lymphoid tissue in the intestinal wall and clusters of lymph nodes. The number of lymphoid follicles increases in the direction from the cecum to the rectum. There are especially many of them in the appendix (appendix) in childhood and adolescence. As we age, lymphatic tissue atrophies.


 (5 ratings, average: 4,40 out of 5)
(5 ratings, average: 4,40 out of 5)