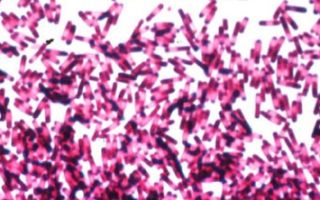
Clostridia (Clostridium) are spore-forming microorganisms that develop in the complete absence of oxygen, feed on dead organic matter and convert organic substances into inorganic ones.
Content
- 1 What is clostridia?
- 2 What to do if clostridia is found in stool?
- 3 Clostridium perfringens
- 4 Clostridium difficile
- 4.1 Why is Clostridium difficile dangerous?
- 4.2 Symptoms of diarrhea and colitis caused by Clostridium difficile
- 4.3 Mild diarrhea caused by Clostridium difficile
- 4.4 Colitis due to Clostridium difficile
- 4.5 Severity of diseases caused by Clostridium difficile
- 4.6 Treatment of Clostridium difficile
- 4.7 Surgical treatment of colitis caused by Clostridium difficile
- 4.8 Prevention
- 4.9 Can Clostridium difficile be cured?
What is clostridia?
Clostridia are widely distributed in soil and water. Some species are pathogenic and cause intestinal infections and many other diseases such as tetanus, gas gangrene, several types of colitis, botulism , etc. If conditions for the development of clostridia are unfavorable, then it forms spores that can persist in the presence of oxygen in the air, dust, on the surfaces of objects, on hands.
Once ingested, clostridia can destroy tissue, which if left untreated can lead to severe complications and even death.
Scientists have found that clostridia poisons have an effect on the human psyche: for example, it is assumed that there is a connection between clostridia and autism. This confirms the danger of clostridia. The positive thing is that healing from clostridia leads to the disappearance of mental symptoms.
Clostridium perfringens is responsible for food poisoning (diarrhea).
Clostridium difficile begins to actively develop in the intestines when the microflora is disturbed, especially often while taking antibiotics.
What to do if clostridia is found in stool?
Clostridium difficile may normally be present in the intestine. According to statistics, it is found in the microflora of 3% of healthy people and 20-40% of hospital patients. In a stool analysis, it should not normally exceed 105 CFU/g. However, if the “health” of the intestinal microflora is disrupted, which especially often happens when taking antibiotics, then clostridia begin to multiply intensively, releasing a potent poison (toxin), which leads at least to diarrhea, but can also cause more serious diseases.
If clostridia is found in feces in acceptable quantities, and there are no other alarming symptoms (diarrhea, nausea, abdominal pain), then you should not resort to drug therapy. In this case, it is necessary to pay special attention to the formation of healthy intestinal microflora.
Clostridium perfringens
These clostridia produce a toxin (poison). The toxin is very persistent and persists even at temperatures of 100 degrees Celsius. Clostridium perfringens causes severe poisoning (gastroenteritis).
How is Clostridium perfringens transmitted?
The infection is most often found in meat and poultry. Infection of people most often occurs due to non-compliance with the technology for preparing and storing large quantities of food.
Clostridia strains that contaminate meat may persist during primary processing. During repeated processing, their spores are formed. During an outbreak of acute infection, up to 70% of those in contact with the infection may become ill.
Symptoms
Symptoms of food poisoning appear 12-24 hours after the contaminated food is eaten.
There are Clostridia perfringens types A and C.
When infected with Clostridium perfringens type A, moderate gastroenteritis develops with the following symptoms:
- stomach ache,
- watery diarrhea.
When infected with Clostridium perfringens type C, necrotizing enteritis with severe symptoms may develop:
- sharp pain in the abdomen,
- bloody diarrhea,
- nausea,
- shock,
- peritonitis.
Diagnostics
The diagnosis is established by the results of an analysis of the culture of Clostridium perfringens in the stool.
Treatment
Type A disease is treated with antibiotics.
In case of development of necrotizing gastroenteritis, urgent surgical intervention is necessary.
Prevention
Prevention of the disease is compliance with sanitary requirements when storing meat, especially in catering establishments.
Can Clostridium perfringens be cured?
In most cases, the disease is completely cured. It is important to start treatment as early as possible to prevent the development of necrosis.
Clostridium difficile
Gastrointestinal discomfort while taking antibiotics is common, but all symptoms disappear when you stop taking the drug. If these symptoms are caused by clostridia, then they not only do not stop when antibiotics are stopped, but may continue for several weeks after discontinuation or even appear only a few weeks after stopping the drug.
Clostridium difficile is spread through direct contact with an infected person, such as through hands or shared objects such as doorknobs, railings, or toilets. Hospital patients are especially susceptible to clostridial infections.
The main symptom is diarrhea. As a rule, it appears 4-9 days after starting antibiotics.
Studies have shown that in patients who stay in a medical hospital for 1-2 weeks, the infection rate is 13%. If patients are in the clinic for more than 4 weeks, then Clostridium difficile is detected in 50% of the people examined.
Recently, this problem has become especially acute, since the incidence of this pathology has increased several times with an increase in mortality from it. In 2009, the European Society of Clinical Microbiologists and Infectious Diseases published its recommendations for treatment, severity and effectiveness of treatment for this infection.
Why is Clostridium difficile dangerous?
Clostridium difficile is an obligate anaerobe and is a gram-positive, spore-forming bacillus with a fecal-oral route of transmission.
This bacillus produces two cytotoxins: A and B.
Toxin A weakens the connection between colonic epithelial cells, which allows toxin B to penetrate between them and trigger a series of inflammatory reactions, including the production of destructive agents and leading to severe tissue damage.
Only in 1978 was it established that Clostridium difficile leads to the development of pseudomembranous colitis that occurs when taking antibiotics.
When taking antibiotics, the intestinal microflora is disrupted. Clostridium difficile spores are acid resistant. Once in the stomach, they penetrate the intestines, where the disturbed microflora does not suppress them. They turn into a vegetative form and begin to produce toxins.
Microbiologists have described a new strain of Clostridium difficile, which produces 16-23 times more A and B toxins compared to previous strains. When infected with this strain, more severe types of disease develop.
Symptoms of diarrhea and colitis caused by Clostridium difficile
Symptoms usually appear 5-10 days after the start of antibiotic treatment, although there are cases of symptoms appearing on the 2nd day of therapy. But it is possible for symptoms to appear 10 weeks after stopping antibiotics.
Typical symptoms of diarrhea and colitis resulting from exposure to Clostridium difficile include:
- profuse offensive diarrhea
- mucus in stool
- cramping abdominal pain
- tenesmus (false contractions)
- occult blood in stool test (sometimes blood in stool)
- leukocytes in feces.
The abdomen is soft, but painful on palpation in the area of the colon.
The disease is characterized by such general symptoms as:
- nausea
- vomit
- dehydration
- moderate fever.
Colitis limited to the right half of the colon is manifested by local abdominal pain, leukocytosis, fever with moderate or mild diarrhea.
The most severe variant of the development of the disease is toxic megacolon. This condition can occur against the background of a decrease in stool, which is sometimes regarded as a positive dynamics of treatment.
However, symptoms such as gas retention, bloating of the colon, high leukocytosis, decreased circulating blood volume, and fluid accumulation in the abdominal cavity are typical manifestations of this condition.
Treatment of toxic megacolon should be surgical.
The severity of the disease depends on the Clostridium difficile strain and the patient's immune status.
Asymptomatic carriage of Clostridium difficile is quite common.
Mild diarrhea caused by Clostridium difficile
A mild form of diarrhea is characterized by the following symptoms:
- moderate abdominal pain
- diarrhea 4 times a day
- absence of general symptoms (nausea, vomiting, fever).
This type of diarrhea caused by Clostridium difficile does not require medication. It is necessary to discontinue antibiotics and prescribe drugs that restore intestinal microflora.
Colitis due to Clostridium difficile
A more severe form is colitis caused by Clostridium difficile. Colitis can occur in the form of colitis without pseudomembranes and in the form of pseudomembranous colitis.
Colitis without pseudomembranes occurs with all the systemic signs of this disease: fever, dehydration, abdominal pain, vomiting, loose, watery stools up to 20 times a day, but without abnormalities in tests.
Pseudomembranous enterocolitis causes the same symptoms, but colonoscopy reveals pseudomembranes and can be confirmed by laboratory abnormalities.
Severity of diseases caused by Clostridium difficile
Guidelines for the diagnosis and treatment of Clostridium difficile-associated diarrhea or colitis provide specific criteria for assessing the severity of this condition.
For ease of perception, they are summarized in a table.
| Severity | Symptoms |
|---|---|
| Mild course | diarrhea up to 5-7 times a day moderate abdominal pain no fever no leukocytosis |
| Moderate to severe | diarrhea 10-15 times a day abdominal pain temperature < 38.5 C moderate dehydration moderate leukocytosis |
| Severe course | hectic fever > 38.5 C severe intoxication circulatory disorders signs of peritonitis signs of intestinal obstruction leukocytosis with a shift to the left presence of pseudomembranes signs of toxic megacolon signs of ascites severe dehydration electrolyte disturbance |
Patients with moderate and severe forms of AAD (antibiotic-associated diarrhea) are subject to mandatory hospitalization.
Treatment of Clostridium difficile
Modern treatment recommendations clearly define the management tactics for patients with AAD (diarrhea) and AAC (colitis).
In a significant number of patients, diarrhea caused by Clostridium difficile is mild.
It goes away on its own after stopping antibiotics and does not require special treatment. Sometimes, in case of dehydration, it is necessary to replace fluids and salts (electrolytes). To replenish fluids and salts, it is recommended to drink plenty of non-carbonated mineral water, unsweetened herbal infusions or special pharmaceutical solutions.
In cases where the disease occurs with obvious signs of colitis, there is a need for antibacterial therapy active against Clostridium difficile.
Criteria for assessing the effectiveness of antibacterial therapy have been determined:
- decrease in stool frequency,
- improving stool consistency,
- improvement of the patient's general condition,
- positive dynamics of clinical and laboratory parameters,
- no new signs of disease progression.
If these criteria are not met, then adjustment of the drug is necessary.
Surgical treatment of colitis caused by Clostridium difficile
Indications for surgical treatment of pseudomembranous colitis are as follows:
- perforation of the colon,
- progression of systemic inflammation with the development of toxic megacolon and intestinal obstruction with adequate antibacterial therapy.
Prevention
- Since the main cause of the development of Clostridium difficile is antibiotics, the main recommendation is the rational use of antibacterial drugs.
- Compliance with sanitary and hygienic standards.
- Isolation of a patient with diarrhea.
- Quick diagnosis.
- Washing hands with soap to remove spores from the surface of the skin.
- Cleaning your hands with alcohol is useless because it does not remove spores.
Can Clostridium difficile be cured?
The prognosis depends on the severity of diarrhea or colitis caused by Clostridium difficile, the nature of the course, and the presence of complications.
In mild to moderate cases, the disease is completely cured. The fever goes away after 1-2 days, and the diarrhea stops after 5-7 days.
Recently, a new effective method of treating even severe cases of the disease has emerged using stool transplantation .
Unfavorable factors are intestinal obstruction , pseudomembranous colitis, and renal failure.