Intestinal infection (or acute gastroenteritis) is a group of acute intestinal infectious diseases caused by the consumption of contaminated foods, with characteristic symptoms of the stomach (lack of appetite, nausea, vomiting) and intestines ( diarrhea of varying severity and abdominal discomfort).
Content
- 1 Causes of intestinal infections
- 2 Types of intestinal infections transmitted by food
- 3 How does infection occur?
- 4 Symptoms
- 5 How does the disease develop?
- 6 Diagnostics
- 7 How to treat an intestinal infection?
- 8 Recovery after an intestinal infection
- 9 Nutrition
- 10 Prevention
- 11 What diseases are classified as intestinal infections?
- 12 Acute intestinal infections in humans
Causes of intestinal infections
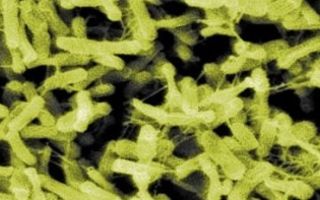
In intestinal infections, poisoning is caused by microorganisms or the toxins they produce.
More often, pathogens of intestinal infections give the name to the disease (for example, salmonellosis - salmonella, botulism - botulinum toxin, etc.). If the intestinal infection that caused the poisoning is not established, a diagnosis of “foodborne toxic infection” or “acute gastroenteritis” is made.
Types of intestinal infections transmitted by food
Foodborne infectious poisonings come in different types.
- Acute poisoning caused by exotoxins (enterotoxins). Toxins produced by some microorganisms interfere with absorption in the intestine and cause increased production of electrolytes (potassium salts, sodium, etc.) and water by the intestine. Although normally these components should be absorbed by the intestines and not excreted. Vibrio cholerae toxins cause especially violent secretion.
- Acute poisoning caused by bacterial toxins that penetrate the mucous membrane of the jejunum and colon . Toxins damage the intestinal wall, causing ulceration, bleeding, secretion (release) of protein, water and electrolytes into the intestinal lumen. This process is observed in diseases caused by Shigella (dysentery), Salmonella and Escherichia coli (hemorrhagic colitis).
- Acute poisonings with little known causes. These include tourist diarrhea.
- Acute infections of non-bacterial nature ( food poisoning ). Poisoning can develop when toxins contained in plants (for example, mushrooms) and food (fish, shellfish) are ingested.
- Gastroenteritis resulting from food intolerance (hypolactasia), food allergies, poisoning with heavy metal salts (arsenic, lead, mercury, cadmium) and side effects of medications.
How does infection occur?
Intestinal infections are not transmitted directly from a sick person to a healthy person. They are transmitted by the fecal-oral route through food. In the case of single diseases, it is not always possible to determine the source of infection. In case of diseases of a group of people, the source of infection can be sick animals, humans or bacteria carriers.
Most often, intestinal infections are transmitted through meat, eggs and processed foods. The probability of infection when they enter the body is high (90% or higher).
Symptoms
The characteristic symptoms of these diseases are:
- nausea,
- vomit,
- complete lack of appetite,
- cramping pain in the abdomen,
- diarrhea, often with blood and mucus.
How does the disease develop?
Poisoning with infectious toxins begins acutely, suddenly. Sometimes the disease is difficult from the very beginning.
Severe dehydration can occur as a result of persistent vomiting and diarrhea. A sudden loss of water in the body can lead to a sharp drop in blood pressure and deterioration of blood supply to organs, which is very dangerous. In addition, oliguria (a sharp decrease in urine production) may develop.
If vomiting causes excessive loss of fluid, then the pH of the blood increases due to the accumulation of alkali, and the content of chlorine and potassium decreases.
Abdominal bloating is common; in severe cases, symptoms of peritoneal irritation appear. of small intestine swollen with gas may be visible through the skin and can be felt by touch.
In laboratory tests in patients with foodborne illnesses in the acute period, changes in the blood (leukocytosis) are observed, but there may also be an increased content of leukocytes, the presence of red blood cells and protein in the urine.
Diagnostics
To establish a diagnosis, the patient’s complaints and identification of symptoms are primary. It is important to find out whether the disease is isolated or a group of people is affected. The next important point to clarify the diagnosis is laboratory data.
Since the disease begins acutely with abdominal pain, it is first necessary to exclude acute diseases of the abdominal cavity.
The diagnosis of “Acute abdomen” is usually not characterized by prolonged diarrhea, and there are no inflammatory changes in blood tests. However, prolonged diarrhea can sometimes be observed with acute appendicitis, partial small bowel obstruction and other acute diseases of the abdominal organs, as well as with colon cancer.
The most significant indicator of intestinal infection is leukocytosis (high white blood cells), and the presence of high eosinophils helps suggest an allergy or parasitic infection.
Suspicious foods, vomit and feces of the patient are subjected to bacteriological examination. Stool testing for bacteria should be carried out no later than 2 days after the onset of symptoms of poisoning.
At the same time, the isolation of a particular microorganism only from material obtained from a patient does not give the right to consider it the causative agent of the disease, since many opportunistic bacteria that cause foodborne toxic infections are often isolated from practically healthy individuals.
Proof that one or another microorganism is the causative agent of a given disease is the identity of the strains isolated from the patient and from suspected products or from several simultaneously ill patients.
Sometimes, using sigmoidoscopy in patients with foodborne toxic infections, erosive-hemorrhagic changes can be detected.
In these cases, it is necessary to check whether the disease is ulcerative colitis or dysentery. Bacteriological examinations of stool, vomit, food, urine and blood help to establish the correct diagnosis.
How to treat an intestinal infection?
Particularly dangerous intestinal infections (for example, cholera, dysentery, etc.) should be treated in infectious diseases hospitals. Less contagious diseases can be treated at home under the supervision of an infectious disease specialist.
Treatment begins with gastric lavage. Lavage is carried out with a gastric tube, regardless of the time elapsed from the onset of the disease. Use a 2% solution of sodium bicarbonate or a 0.1% solution of potassium permanganate in a volume of at least 3 liters.
For mild food infections, when nausea or vomiting has stopped, a glucose-electrolyte solution is prescribed orally, containing in 1 liter of boiled water sodium chloride - 3.5 g, sodium bicarbonate - 2.5 g, potassium chloride - 1.5 g, glucose - 20 d. You can use ready-made preparations “Regidron” and “Glucosalan” in packages.
In severe cases, infectious-toxic shock, uncontrollable vomiting and severe dehydration, glucose-elerolyte solutions are administered intravenously. Polyionic solutions “Trisol”, “Chlosol”, “Kvartasol” are used. If fluid loss reaches 7-10% of body weight, then the solutions are injected in a stream at a speed of 80-120 ml/min.
For severe vomiting, antiemetics such as dimenhydrinate, prochlorperazine, promethazine, trimethobenzamine can be used intramuscularly or as enemas.
Antibiotics have a quick effect, but their use can cause dangerous damage to the intestinal mucosa. In this regard, it is better to use sulfonamides (Biseptol) or halogen-containing hydroxyquinolines (Intetrix) for 5-7 days.
To reduce diarrhea, adsorbents, enveloping and anti-inflammatory agents (medicinal charcoal, pectins, etc.) have a good effect.
Apples contain a large amount of pectin. In this regard, in mild cases, grated apples can be used as an antibacterial agent in the amount of 1 kg per day in combination with oatmeal and ascorbic acid.
Medical charcoal is prescribed in a dose of 1 to 4 tablets up to 3 times a day, each time after loose stools.
To eliminate diarrhea, you should not use antidiarrheal drugs, as they contribute to the retention of pathogenic microbes and toxins in the body, and in case of severe disturbances of intestinal tone, they can cause dynamic intestinal obstruction.
Recovery after an intestinal infection
The prognosis for intestinal infections is favorable, mortality ranges from 0.04 to 0.6%. Full recovery does not occur immediately.
The period of complete recovery may last several weeks or even months.
Patients are concerned about weakness, asthenia, sweating, tachycardia. Functional disorders of the stomach and intestines are often observed in the form of alternating diarrhea and constipation (either diarrhea or constipation), flatulence, abdominal pain, poor tolerance to milk and other products containing disaccharides.
Patients who have suffered foodborne toxic infections often experience disturbances in the motor, digestive and absorption functions of the intestine for a long time. Taking into account the simultaneous dysfunction of the autonomic nervous system, asthenia and apathy, dysfunction of internal organs can become the basis for the further formation of neuroses and persistent functional diseases of the digestive system, for example, irritable bowel syndrome.
Nutrition
For intestinal infections in the acute period, diet 4b , during the recovery period diet 4c.
Prevention
Prevention of food toxic infections consists of observing sanitary and hygienic standards for storing and transporting food products, eating high-quality canned food and products, water, and maintaining personal hygiene.
What diseases are classified as intestinal infections?
The main types of infectious intestinal diseases, the causative agents of which have been identified, include:
hemorrhagic colitis (bloody diarrhea),
Acute intestinal infections in humans
| Pathogen | Disease | Symptoms |
|---|---|---|
| Shigella | Bacterial dysentery | Fever, diarrhea, stool culture positive for Shigella |
| Salmonella | Bacterial dysentery, acute gastroenteritis | Fever, diarrhea, stool culture positive for salmonella |
| Yersinia | Yersinia enterocolitis (yersiniosis) | Abdominal pain, diarrhea (usually bloody), fever, stool culture positive for Yersinia |
| Campylobacter | Bacterial dysentery | Fever, diarrhea (often bloody), stool culture positive for Campylobacter |
| The causative agent of lymphogranuloma venereum | Proctitis | Pain in the perineum during defecation. Serological tests and stool bacterial culture for Chlamydia trachomatis are positive |
| Chlamydia | Proctitis | Involvement of lymph nodes, homosexuals are more likely to suffer, positive serological tests |
| The causative agent of gonorrhea | Proctitis | Diarrhea. Detection of gonococci in rectal discharge. |
| Clostridia | Pseudomembranous colitis | Diarrhea due to antibiotic treatment |
| Tuberculosis bacillus | Intestinal tuberculosis | Abdominal pain, diarrhea, fever, blood in the stool, possible combination with pulmonary tuberculosis. Tuberculin tests are positive. Koch bacilli can be cultured from sputum and feces. |
| Cytomegalovirus infection | HIV infection | Polysystemic manifestations. Positive reaction to HIV infection. |