Dysentery (shigellosis) is an intestinal infection caused by one of four types of Shigella with predominant damage to the mucous membrane of the distal colon ( sigmoid and rectum).
Content
What is dysentery?
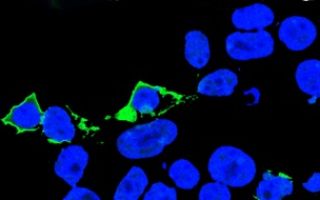
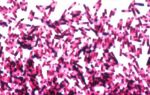
The disease develops when Shigella enters the body. Since these bacteria are rod-shaped microbes, they are also called dysentery bacillus. First, active development of microbes occurs in the small intestine, followed by penetration into the epithelium of the colon. Shigella penetrates epithelial cells, multiplies in them, spreads along the intestine, causing cell death, which leads to intestinal swelling and the formation of ulcers.
At the same time, Shigella secretes toxins (poison), which also cause cell death and stimulate increased intestinal secretion of water and electrolytes (sodium, potassium salts, etc.), and also have a specific effect on the nervous system and the functioning of the adrenal glands. Toxins cause general severe poisoning of the body.
How does infection occur?
Sources of dysentery infection are patients and bacteria carriers, contaminated products. The disease is transmitted by the fecal-oral route (by mouth only).
Conventionally, the transmission routes of dysentery can be divided into household , food and water .
Household infection occurs through direct contact with a patient, through common objects (door handles, switches, etc.)
Dysentery bacilli released into the external environment can persist in water, soil, food products, and on the surface of various objects from several days to several months.
Cases of dysentery occur all year round, but the number usually increases in summer and autumn. Flies transmit dysentery bacteria to food.
Consumption of contaminated food without thermal and hygienic treatment can cause group disease.
Infection can occur from drinking contaminated drinking water and from swimming in open water.
The most dangerous are patients with mild dysentery. Due to mild symptoms, these people do not seek medical attention, but are highly contagious.
Symptoms
Most often, bacterial dysentery is acute, but cases of chronic form also occur if the disease lasts more than 3 months.
The disease appears 3-4 days after infection (incubation period).
Symptoms of acute dysentery
Acute dysentery goes through two phases in its development:
- the first phase is small intestinal,
- the second phase is colonic.
When active Shigella development occurs in the small intestine, it is manifested by the following symptoms:
- fever,
- pain in the upper abdomen,
- copious fecal stools.
When the process spreads to the large intestine, signs such as:
- loose mucous stools,
- blood in stool
- mucus and pus in stool,
- false painful urge to defecate (tenesmus),
- stool up to 20-50 times a day,
- cramping pain in the abdomen.
At the same time, during the second phase, the temperature normalizes, abdominal pain moves to the lower abdomen. If treatment is started in time, the disease may be limited to one phase.
Due to loss of fluid and lack of appetite, the patient quickly loses weight, facial features become sharper, the skin becomes dry, and the limbs become cold. Thirst appears.
The severity of the disease depends on the person’s age and health status. Dysentery can manifest itself as mild diarrhea, or a severe form with dehydration, and even dystrophy. Severe disease is rare and occurs mainly in children, old people and people with weakened immune systems.
Symptoms of chronic dysentery
Chronic dysentery occurs in the form of abdominal pain, loose stools mixed with mucus and blood, and false urges several months after apparent recovery.
The development of chronic dysentery is promoted by vitamin deficiency, general weakening of the body, exhaustion, and overwork.
Exacerbations are caused by poor diet, stress, and consumption of foods rich in fiber.
Patients with chronic dysentery play an important role as a source of infection for others.
Complications
With dysentery, a complication is possible that occurs 1-4 weeks after the onset of diarrhea. This complication is called Reiter's syndrome after the German doctor who described it.
The complication occurs suddenly, the body temperature rises sharply, weakness and a complete lack of appetite appear. Eczema appears on the skin, and less commonly, herpes. A clear sign is inflammation of the mucous membranes (conjunctivitis, urethritis).
This is often accompanied by stomatitis, rhinitis, bronchitis, cystitis, and pharyngitis. Inflammation of the joints (arthritis, tendovaginitis), meninges (meningitis), and pleurisy is also possible. Sometimes there are systemic lesions of the liver, kidneys, salivary and lymph glands.
The course of this complication is chronic, with exacerbations. This disease leads to weight loss, disruption of the structure of hair, nails, and skin changes.
Most often, this syndrome develops in men aged 20 to 40 years.
Diagnostics
In any case of diarrhea with fever, you should consult a doctor to rule out dysentery.
Inflammatory processes in the intestines are indicated by a large number of red and white blood cells. A final diagnosis can only be made if Shigella is detected in stool cultures.
Treatment
Mild forms of dysentery can be treated at home under the supervision of an infectious disease specialist, subject to strict adherence to sanitary and hygienic standards.
- The patient's stool must be disinfected. They should be covered with dry bleach, left for an hour and only then discharged into the sewer.
- After each use, boil the patient’s dishes in a 2% soap-soda solution (1.5 tablespoons of baking soda per 1 liter of soap solution).
- Boil underwear and bed linen in a soap-soda solution for 30 minutes.
- You can use ready-made medical solutions for disinfection.
- Carry out wet cleaning of the premises daily.
In case of severe dysentery, treatment must be carried out in a medical facility.
Treatment of acute dysentery
The basis of treatment is rehydration of the body (replenishment of lost fluid and salts), vitamin therapy and diet therapy. It is recommended to drink ready-made solutions of glucosalan and rehydron. In addition, you need to drink non-carbonated mineral water and unsweetened herbal teas.
It is recommended to eat for dysentery according to the 4-4b therapeutic diet .
Medicines are used to reduce fever and shorten the period of bacterial carriage.
In severe cases, older people are prescribed antibiotics.
Antidiarrheal drugs should not be used, as they contribute to the retention of Shigella in the intestines.
home remedies to reduce diarrhea .
Treatment of chronic dysentery
For chronic dysentery, strict adherence to the diet is necessary (diet 4b-4c is recommended).
For exacerbations, antibiotics, digestive enzymes and astringents are prescribed.
A course of antibacterial therapy must be combined with vaccine therapy. The vaccine is administered subcutaneously.
In case of complications (Reiter's syndrome), treatment is aimed at eliminating inflammatory processes.
Is it possible to be cured?
With timely and correct treatment, complete recovery occurs. , irritable bowel syndrome may develop .
With chronic dysentery and complications, the prognosis is uncertain, since after a period of normal health, an exacerbation may occur again.
Prevention
The prevention of dysentery is facilitated by strict adherence to sanitary standards and personal hygiene.
If there is a sick person in the house, then to avoid contracting dysentery, you should:
- isolate his dishes and household items,
- disinfect all common areas,
- fill the patient’s secretions with disinfectant solutions and only then pour them into the sewer system,
- Wash bed and underwear separately at temperatures above 60 degrees.
In the summer, careful processing of products and protection of products from flies is necessary.